Lower Back Pain
Different therapists will offer their method of treating lower back pain but for patients it can be difficult to know what is right for them. Many of these proposed treatments are not supported by science and either based on theory or anecdotal. Thankfully, the research for both chronic and lower back pain has come a long way. I have been delving into some of these studies and it is encouraging news for most of us! There are some excellent clinicians in the physiotherapy world who are leading the research on pain science and lower back pain. Although pain mechanisms in the lower back pain can be based on many factors, the science now helps us to understand their role and how to manage them. In this blog I will summarize the current research and how this changes the treatment approach.
Lower back pain research update.
I am going to summarize the most important research as this has a direct impact on how lower back pain should be treated.
- Most lower back pain involves a minor sprain from a mechanical loading injury. Sometimes it is a pain flare-up caused by a sensitized nervous system, with some psychosocial and lifestyle factors being the main drivers of pain. Pain can be amplified by the brain with lack of sleep; stress and anxiety; fearful/catastrophizing thought patterns about pain and injury; and lifestyle factors. The take home message here is that none of these pain drivers are related to structural damage in the spine. Only about 1-2% of patients will have a serious systemic diagnosis requiring further medical attention. Only about 5-10% of patients will have a serious neurological problem requiring diagnostic imaging and referral to a specialist.
- For patients with disc herniations and sciatica symptoms the natural history of recovery is good. About 80% will recover by the end of 12 months. Only a small percentage will need surgery due to progressive neurological symptoms. Most disc bulges and herniations will resolve over time with careful pain management. Encouraging movement in the spine and the nerves will desensitize the nervous system and tell the brain it is safe to move.
- Interestingly, studies have shown that a high percentage of patients who have lower back pain show no signs of anything on an MRI. Conversely, other MRI studies show that people with no lower back pain have disc bulges, protrusions and herniation. We also know from recent pain research that pain does not correspond with tissue damage and there are a number of another factors that can amplify a pain response. The take home message from all of this is that MRI’s can be misleading, causing unnecessary worry and do not represent the complete clinical picture. Unnecessary imaging can actually increase pain through fear of movement which then becomes a movement dysfunction.
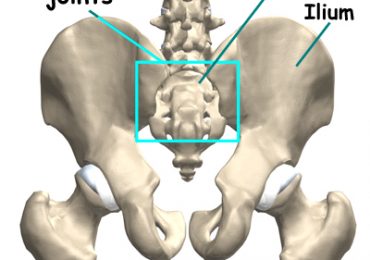
- There is growing evidence that psychosocial stressors can amplify pain. The brain can centrally increase pain perception when the initial painful stimulus in the lower back is minimal. These psychosocial stressors include sleep disturbance; prolonged stress; anxiety and depressed moods. Negative thoughts of catastrophizing and fear about lower back pain are predictive of higher pain levels, more chronicity and disability. Some of these negative thoughts turn into pain behaviours, where patients try to adapt their movements to pain or avoid certain ones altogether. Pain is not a good indicator of tissue damage. The spine and pelvis are actually quite stable structures and we know the pain is more related to sensitivity of the nervous system and regulated in the brain.
- There has never been any research that shows a relationship between lower back pain and weak/unstable core. In fact the whole idea of weak and unstable core is based on theory. No studies have ever shown that our spine and pelvis are unstable. Recent studies with lower back pain subjects showed that there was no difference between groups doing core exercises and general back exercises. The research into the core muscles of the lower back and abdomen only showed there was a delay in timing with lower back pain. The timing was a fraction of a second and it did not show that it caused instability or weakness. Many lower back pain patients already have too much co-contraction, exactly what core strengthening aims to achieve. Encouraging patients to brace and restrict normal movement creates faulty movement patterns.
Evidence Based Treatment for Lower back Pain.
- Patients need to be assessed for these psychosocial drivers of pain. It doesn’t mean you have to go to a mental health professional as many of these factors can be identified in a thorough physiotherapy assessment. Some of the advice and management around pain is part of the physiotherapy treatment. Fears around movement can be addressed by encouraging safe movement in the direction of pain. The Pilates equipment allows a variety of ways to unload painful areas of the spine so that movement can be restored. Patients are given the correct messages about pain and movement so that the brain does not register these as a threat. The key here is not about strengthening the back or creating more stability. It is about desensitizing the painful stimulus in the back and also the central brain drivers of pain.
- A treatment session should address any cognitive barriers to movement as discussed. Then the incorrect movement patterns can be addressed by normalizing the mechanics of the spine. Acute episodes of lower back pain need to be protected more with cautious movement into the pain. More chronic pain over 3 months will have more psychosocial factors involved as these will be barriers to normal movement. Safe supervised movement using the Pilates equipment is ideal as it directly grounds the fear and negative thoughts about moving. Some of the more general psychosocial drivers of pain can be alleviated with advice and education on self-management. Treatment is about gradually exposing the spine to normal movement and having patients understand it is safe and harmless.
Damian Wyard is a registered physiotherapist in Downtown Toronto. He combines Pilates and physiotherapy in supervised rehabilitation for lower back injuries and conditions. Supervised sessions on the classic Pilates equipment are a great way to start the recovery process and eventually patients self-manage with home programs. Damian is particularly invested in updating treatments based on the latest research. Patients come with a range of lower back conditions as well as post-surgery cases such as discectomy.